The Intricate Dialogue Between the Brain and Immune System: Unraveling Neuroimmune Crosstalk
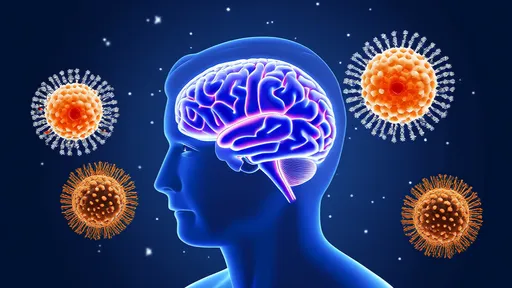
For decades, the central nervous system (CNS) and immune system were studied as separate entities, operating in isolation with distinct functions. The brain was considered an immunologically privileged site, shielded by the blood-brain barrier, while the immune system patrolled the periphery. However, groundbreaking research over the past two decades has shattered this dogma, revealing an astonishingly sophisticated bidirectional communication network that fundamentally links neural circuits with immune responses.
This neuroimmune crosstalk represents one of the most transformative discoveries in modern medicine. We now understand that the CNS doesn't merely receive immune signals but actively shapes immunological outcomes through multiple pathways - neural, endocrine, and even direct cellular contacts. Conversely, immune cells and their molecular messengers can dramatically influence neural function, behavior, and even cognitive processes. This paradigm shift has opened new frontiers in understanding conditions ranging from depression to neurodegenerative diseases.
The anatomical basis of this interaction is remarkably elegant. The vagus nerve, the longest cranial nerve connecting the brain to major organs, serves as a superhighway for immune-to-brain signaling. When immune cells detect infection or injury in peripheral tissues, they release cytokines that activate vagal sensory fibers. These signals reach the nucleus tractus solitarius in the brainstem within milliseconds, triggering neuroinflammatory responses that often precede detectable changes in blood cytokine levels.
Meanwhile, the CNS exerts top-down control through both the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. Glucocorticoids released during stress responses can suppress certain immune functions, while norepinephrine from sympathetic neurons modulates immune cell activity in lymphoid organs through adrenergic receptors. Recent single-cell sequencing studies reveal that nearly all immune cell subtypes express receptors for neurotransmitters, highlighting the evolutionary importance of neural regulation.
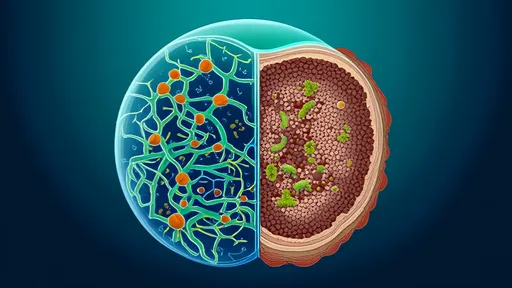
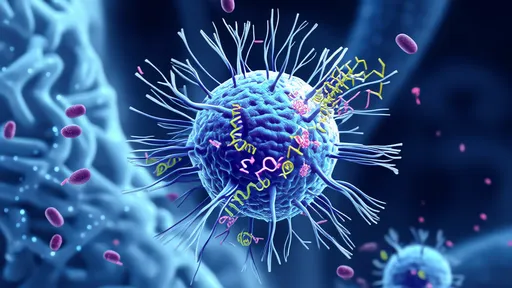
Microglia, the resident immune cells of the brain, have emerged as central players in this dialogue. Once considered simple scavengers, these dynamic cells constantly survey the neural environment, pruning synapses in development and responding to disturbances with remarkable precision. Their activation states are directly influenced by neuronal activity patterns through purinergic signaling and fractalkine pathways. Conversely, microglia release growth factors and inflammatory mediators that shape neural circuit function, creating a continuous feedback loop.
The implications of disrupted neuroimmune communication are profound. In major depressive disorder, elevated pro-inflammatory cytokines can access the brain through active transport mechanisms and volume diffusion at circumventricular organs. These immune molecules alter monoamine metabolism, reduce neurotrophic support, and contribute to the sickness behaviors that overlap with depression symptoms. Similarly, in Alzheimer's disease, chronic microglial activation driven by amyloid pathology may transition from protective to neurodegenerative over time.
Remarkably, the immune system appears capable of forming something akin to immunological memory of neural activity patterns. Animal studies demonstrate that prior exposure to certain stressors can prime neuroinflammatory responses to subsequent challenges, a phenomenon termed "neuroimmune sensitization." This may explain why some individuals develop mood disorders after minor immune triggers while others remain resilient. The molecular mechanisms involve epigenetic modifications in both immune cells and neurons that persist long after the initial stimulus resolves.
Cutting-edge therapeutic approaches are harnessing this knowledge. Vagus nerve stimulation, already FDA-approved for epilepsy and depression, shows promise in rheumatoid arthritis and inflammatory bowel disease by activating the cholinergic anti-inflammatory pathway. Conversely, anti-cytokine therapies developed for autoimmune conditions are being repurposed for treatment-resistant depression with encouraging results. Perhaps most intriguing are efforts to develop "neuroimmune modulators" - drugs that specifically target the interface between these systems without broadly suppressing either.
The gut microbiome adds another layer of complexity to this conversation. Gut microbes produce neurotransmitters and metabolites that influence both systemic immunity and CNS function through the vagus nerve and circulatory system. The emerging gut-brain-immune axis suggests that many neurological conditions may benefit from interventions targeting microbial communities. Fecal microbiota transplantation has shown remarkable effects in animal models of multiple sclerosis, while specific probiotics demonstrate anti-inflammatory and anxiolytic properties.
As research progresses, we're discovering that neuroimmune interactions operate across vastly different timescales. While some signals, like noradrenergic activation of splenic immune cells, occur within seconds, others unfold over years - such as the gradual neuroinflammatory processes contributing to Parkinson's disease pathology. This temporal dimension adds considerable complexity when designing interventions, as the therapeutic window and approach may differ dramatically depending on disease stage.
The clinical ramifications extend beyond neurology and immunology. Cancer immunotherapy responses appear influenced by stress-related neural signaling, while post-stroke cognitive decline correlates strongly with peripheral immune activation patterns. Even in conditions like long COVID, where patients experience persistent neurological symptoms, dysregulated neuroimmune communication is increasingly implicated. These connections suggest that future medical specialties may need to adopt more integrative approaches to patient care.
Technological advances are propelling the field forward at an unprecedented pace. High-resolution imaging now allows visualization of neuroimmune interactions in living organisms, while optogenetic tools enable precise control of specific neural circuits to study their immunological effects. Meanwhile, multi-omics approaches are revealing how genetic variants associated with neurological and immunological diseases often converge on shared biological pathways.
Despite these exciting developments, significant challenges remain. The blood-brain barrier, while permeable to immune signals, presents formidable obstacles for drug delivery. The pleiotropic nature of cytokines means that manipulating one mediator can have unpredictable ripple effects across multiple systems. Furthermore, individual differences in neuroimmune regulation may explain why some therapies work brilliantly in certain patients but fail in others, underscoring the need for personalized approaches.
Looking ahead, the neuroimmune perspective promises to revolutionize how we understand health and disease. By appreciating the brain not as an isolated command center but as an integrated component of systemic physiology, constantly conversing with our defenses, we may unlock new strategies for promoting resilience and treating complex disorders. The next decade will likely see neuroimmunology transition from a specialized field to a fundamental pillar of biomedical science, reshaping medical education and clinical practice in its wake.
By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025
By /Jun 19, 2025
By /Jun 19, 2025

By /Jun 19, 2025